This content is based on the British Columbia Mental Health and Wellness Recovery Toolkit.
This tool kit provides practical guidance and resources to authorities, organizations, and agencies involved in community mental health programs and services. It helps plan and deliver support for community recovery after disasters.
Psychosocial supports and services
Anyone who experiences a crisis may need psychosocial support.
For many, the care and support of family, friends, or the community eases short-term distress. Some people may need professional care, and a few may require specialized mental health services.
Recognizing these differences helps determine the right support or interventions.
Activation of community-led support
After a large disaster, certain mental health and wellness services are considered best practices. These are divided into four phases: immediate, short-term, medium-term, and long-term.
The Mental Health and Psychosocial Support (MHPSS) Intervention Pyramid, described below, outlines each phase’s activities. Recovery times vary by event and community, so the suggested timeframes are only guidelines.
Also, bear in mind that supports like primary care, mental health, and substance use services can be used throughout the recovery process.
Phases of intervention
This tool kit follows the Mental Health and Psychosocial Support Intervention Pyramid (MHPSS Intervention Pyramid), described below.
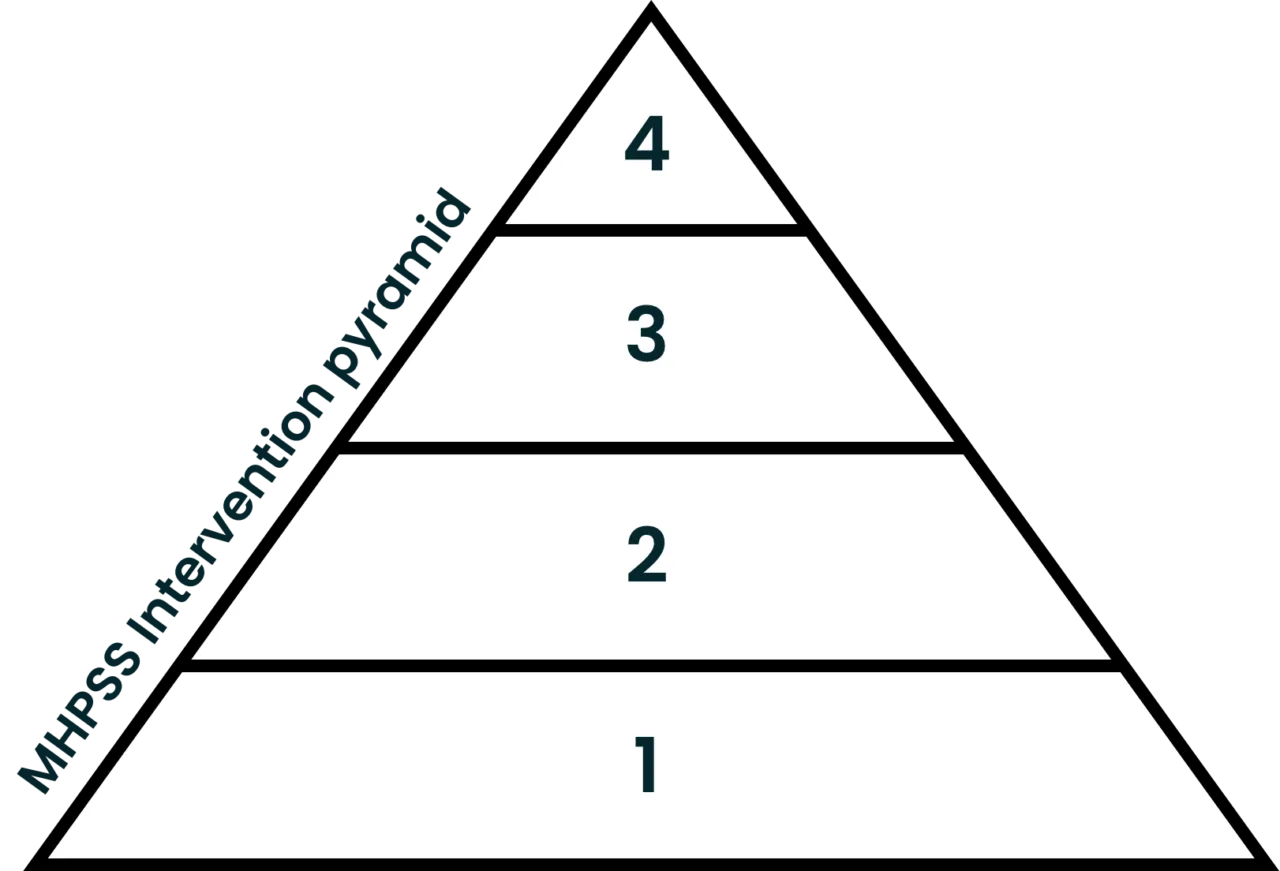
- Basic services and security: The most basic response in the aftermath of a disaster. Psychological First Aid (PFA)–trained responders provide support, calm, and stabilization in the hours, days, and weeks following the event.
- Community- and family-strengthening supports: Focuses on community services and family supports aimed at improving coping and promoting recovery (e.g., strength-based skills interventions).
- Focused, non-specialized supports: Refers to more focused supports and psychoeducation interventions for individuals and families. Typically provided by practitioners working in primary care, mental health, and community-based settings.
- Specialized services: Includes specialized clinical services for the small percentage of the population experiencing more severe symptoms of depression, anxiety, and PTSD, as well as pre-existing difficulties with mental health and complex substance use.
- Immediate
- Short-term
- Medium-term
- Long-term
Phase 1: Immediate aftermath
What to do in the days following a disaster
Right after a disaster, people focus on keeping themselves and loved ones safe. They need shelter, food, health care, and other urgent support. Meeting these needs helps restore calm and security.
Suggested activities and services
| Activities and services | Target populations | Service providers |
|
|
|
Three main actions to put in place
- Collaborate with the Emergency Operations Centre (EOC) to:
- Ensure community members benefit from basic services (e.g., food, housing, medical care).
- Spread important information through the media, such as crisis line numbers, coping tips, etc.
- Form a local Mental Health and Wellness Working Group (MHWWG) to determine local needs, provide psychological support, and strengthen overall resilience.
- Conduct a rapid needs assessment with information from your initial working group, EOC reports (e.g., types/numbers of those impacted), additional reports from responding First Nation governments or local authorities, and NGOs.
Additional resources
For more details about Psychological First Aid (PFA) and immediate community assistance in the days after a disaster, visit:
For more details about how to communicate with your community in the context of a disastrous event, visit:
Phase 2: Short-term aftermath
What to do 1–6 months following a disaster
In the first six months after a disaster, it is important to keep sharing mental health information with those affected. This information should offer tools to manage stress, build coping skills, and focus on self-care. It should also include ways to access support, like crisis lines and counseling. Providing these resources helps restore a sense of safety, especially for children and youth.
Suggested activities and services
| Activities and services | Target populations | Service providers |
|
|
|
Four main actions to put in place
- Ensure the MHWWG continues to meet regularly.
- Conduct a community needs assessment to determine short-, medium-, and long-term recovery needs and priorities.
- Promote community activities and ensure meeting places are available.
- Keep identifying vulnerable populations and local services that can support them.
Additional resources
For more details about emergency management and the role of the MHWWG, visit:
For coping resources, activities, and services to share with affected survivors, visit:
Phase 3: Medium-term aftermath
What to do 7–12 months following a disaster
Between seven and twelve months after a disaster, recovery may become harder. People might feel more exhausted, depressed, or anxious. Some may turn to substances or experience family violence. To help, mental health programs and training should match the community’s needs. Smaller communities may need outside support, which the MHWWG can request.
Suggested activities and services
| Activities and services | Target populations | Service providers |
|
|
|
Three main actions to put in place:
- Continue MHWWG meetings to track the community’s status, local resources, and needs for extra support or training.
- Work with local government recovery teams and provincial or territorial groups to share updates on mental health needs and available support.
- Plan events like commemoration or wellness days to recognize community resilience, thank helpers, and promote strength.
Additional resources
For information sheets and helpful resources directed to bereaved survivors:
For information about how parents can help their children deal with bereavement:
For a list of Canada’s national crisis lines, visit this page on our website.
Phase 4: Long-term aftermath
What to do 12–36 months and more following a disaster
Many people recover from a disaster without needing mental health services, but some require extra support. Symptoms may appear months or even years later, and recovery can take anywhere from a few years to a decade. Level 4 of the MHPSS Intervention Pyramid focuses on the 4–5 percent of people most affected, who show severe symptoms linked to major mental health conditions like depression, anxiety, or PTSD. Support options include:
- Outpatient mental health and substance use treatment.
- Inpatient care for severe mental health and substance use issues.
- Medication to help manage mental health symptoms.
- Therapy from psychiatrists, psychologists, or trained general practitioners.
Suggested activities and services
| Activities and services | Target populations | Service providers |
|
|
|
Three main actions to put in place
- Develop an annual status report (MHWWG) to highlight successes, ongoing efforts, and remaining needs. This report should formally update local and provincial governments and request extra support if needed.
- Organize community commemoration and wellness days (developed in Phase 3) to strengthen community bonds, promote health, recognize resilience, and thank helpers and recovery teams.
- Continue sharing mental health information to reduce stigma, raise awareness about long-term disaster effects, and inform people about available support options.
Additional resources
For additional information about PTSD and helpful fact sheets for survivors of disasters, visit:
